Our Approach
Rooted in TCM and coupled with the knowledge of the most recent scientific research, Kidney Health Institute has developed a strong expertise in helping patients with Chronic Kidney Disease (CKD) to improve their kidney condition and ameliorate its complications, using a holistic approach that includes all-natural Chinese herbal treatment and other natural therapies.
The practitioner will analyze each patient’s unique history, severity of the condition, and overall health to make a customized treatment plan, which will help patient restore their kidney structure and function, repair kidney damage, and addresses various CKD complications. Patients can experience improvement within a short period of time such as an increased energy level, better appetite and sleep quality, reduced swelling and bubbling of urine. As the patient continue the treatment, their kidney structure and function will continue to be restored, which will be reflected in their blood test results such as BUN and creatinine level.
The reason why our treatment gives patients satisfactory results is our holistic approach that addresses the root cause of CKD, which is critical due to the many impacts CKD has on patient’s health. Drawing from more than 10 years’ experience, our staff practitioners will provide you with an optimal plan to get your life back on track.
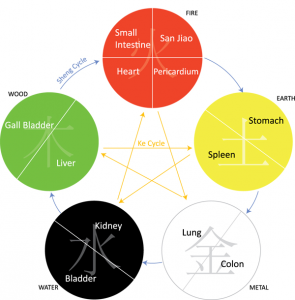 Traditional Chinese Medicine (TCM) is based upon the premise of balance between the body’s core organs and the structure (Yin) and function (Yang) within each organ. The relationship between these organs and the Yin/Yang within each organ is not completely understood, but scientific evidence has come to support many of the ancillary assertions of TCM such as the direct impact that specific naturally occurring compounds have on the regulation of the organ’s activities.
Traditional Chinese Medicine (TCM) is based upon the premise of balance between the body’s core organs and the structure (Yin) and function (Yang) within each organ. The relationship between these organs and the Yin/Yang within each organ is not completely understood, but scientific evidence has come to support many of the ancillary assertions of TCM such as the direct impact that specific naturally occurring compounds have on the regulation of the organ’s activities.
High Blood Pressure
The kidneys play a vital role in long-term blood pressure regulation. Several factors associated with CKD can contribute to the increased blood pressure in CKD patients. First of all, damage of the tiny filtering units in the kidneys will result in retention of salts, wastes and extra fluid in the blood. Such extra fluid build-up in the blood vessels can raise blood pressure. Second, impaired sodium excretion in the kidney can cause increased peripheral resistance. Although the exact mechanism remains unclear, experiments has found that in a series of patients with renal failure due to histologically proven hypertensive nephrosclerosis, transplant with kidneys from normotensive donors resulted in the resolution of their hypertension.
Excess amount of renin produced by the failing kidneys due to the stimulation by the increased sympathetic nervous activity in CKD patients can cause over activation of the renin-angiotensin system (RAS). It has been found to be the cause of uncontrolled hypertension despite optimized ultrafiltration in dialysis patients. Other factors include reduced generation of vasodilators such as nitric oxide and kinins; and imbalance between vasodilator and vasoconstrictor prostaglandins[1].
Angiotensin-converting enzyme (ACE) inhibitors and angiotensin receptor antagonists are the common drugs used in CKD patients to control their blood pressure. However, both of these drug classes can cause a decrease in Hb concentration in patients with diabetes and CKD. These drugs can directly block the proerythropoietic effects of angiotensin II on red cell precursors, degradation of physiological inhibitors of hematopoiesis, and suppression of IGF-I. Iosartan, a blood pressure medication used for renoprotection, can lower Hb by ∼1 g/dl after long-term administration in 50- to 100-mg doses once daily in patients with diabetes and CKD. It should be recognized that these classes of agents may induce or worsen symptomatic anemia in nephropathy patients[2].
Using Chinese herbal formulas, Kidney Health Institute Practitioners can help CKP patients reduce their high blood pressure into a normal range.
- Patients can experience their improved blood pressure within 2-4 weeks of treatment.
- With 6 weeks to 3 months treatment, patients can reduce or stop taking their blood pressure medication while maintaining their blood pressure in the normal range.
High Blood Sugar
While diabetes can cause CKD, it is also a common complication of CKD. Patients with CKD have a decreased insulin secretion by the pancretic β -cell and resistance to insulin in their liver and muscle cells. When glomerular filtration decreases below 50 ml/min insulin secretion will be decreased caused by metabolic acidosis and the elevation of intracellular calcium concentration and decrease of the cellular content of ATP and Na-K-ATPase pump activity in the pancreatic β cells [3].
Patients with renal failure have impaired insulin sensitivity with consequent abnormal glucose levels due to an increase of gluconeogenesis in the liver, reduction of glucose uptake, and impaired glycogen synthesis in the liver. The cause of such insulin resistance is uremia toxins in CKD patients. Decreased tissue oxygen delivery because of anemia also contributes to insulin resistance in uremia 3.
Using Chinese herbal formulas, Kidney Health Institute practitioners can help CKD patients reduce their blood sugar down effectively into a normal range measured by fasting glucose level and HA1C.
- With 2-4 weeks of treatment, patients can experience improved blood sugar levels.
- With 6 weeks to 3 months treatment, patients can reduce or stop taking their blood sugar medication or insulin while maintaining their blood sugar in the normal range.
Anemia
Anemia is a condition characterized by a reduction in red blood cell. The prevalence of CKD-associated anemia is approximately 50%. The major causes of anemia in CKD patients are decreased erythropoietin syntheses. Erythropoietin is a glycoprotein secreted by the kidney interstitial fibroblasts and is essential for the growth and differentiation of red blood cells in the bone marrow. In CKD, tubular atrophy and tubulointerstitial fibrosis compromises renal erythropoietin synthetic capacity and results in anemia.
Anemia can cause physical and mental dysfunction with symptoms of malaise, fatigue, weakness, dyspnea, impaired cognition, and other symptoms such as impaired sexual function. In CKD patients complicated with diabetes, anemia can contribute to retinopathy, neuropathy, or diabetic foot ulcer. Anemia can directly cause further progression of kidney disease. Renal ischemia due to reduced oxygen worsen renal medullary hypoxia, leading to renal interstitial injury and fibrosis. Anemia also causes increased renal sympathetic nerve activity, resulting in increased glomerular pressure and proteinuria which in turn accelerates progression of kidney disease2.
Under anemia conditions, the heart contracts harder to meet the body’s oxygen demand. Over time it causes left ventricular hypertrophy (LVH) and heart failure. Heart failure causes further renal function deterioration and leads to a vicious cycle termed the “cardiorenal anemia syndrome” which significantly increases morbidity and mortality of CKD patients.
Using Chinese herbal formulas, Kidney Health Institute Practitioner can help patients nurture the blood and enhance red blood cell production from the bone marrow.
- With 2-4 weeks of treatment, patients can experience improvement in anemia related symptom
- With 4-6 weeks of treatment, patients can have sustained increase of red blood cell count
Cardiovascular Complications
Over 50% of CKD patients are likely to die from cardiovascular disease. End-stage CKD patients and dialysis patients have eight times the mortality rate of their age-matched counterparts in the general population.
CKD patients can develop several types of heart conditions. Since the heart condition develops over a long period of time, patients can be asymptomatic. As the heart related symptoms overlaps with CKD, their heart condition can be easily overlooked in their treatment.
Congestive Heart Failure
Congestive heart failure (CHF) is found in about one-quarter of cases of chronic kidney disease. The prevalence of congestive heart failure increases greatly as the patient’s renal function deteriorates, and, at end-stage renal disease, can reach 65-70%. Chronic kidney disease is a major contributor to severe cardiac damage and, conversely, that congestive heart failure is a major cause of progressive chronic kidney disease[4].
Pericarditis and pericardial effusions
Pericarditis and pericardial effusions are common complications among end-stage CKD patients. Statistic studies shows that 30% of pericardial effusions is caused by cancer and 22% of pericardial effusions is caused by CKD. Although the pathogenesis is poorly understood, it is found that pericarditis is related to uremic toxins. Uremic pericarditis is correlated to the degree of azotemia especially when the BUN is >60mg/dL (normal is 7-20 mg/dL). The incidence has been analyzed and in one of the study involved with 83 patients admitted to the chronic dialysis program uremic pericarditis was occurred in 41% [5][6].
Using echocardiography the incidence of pericardial effusion can be accessed. Studies on a group of 41 stable asymptomatic patients on chronic haemodialysis found that 21 (51%) of them had developed pericardial effusions. Out of 21 patients with echocardiographic effusions, 15 of 41 (37%) of those had more than 100 ml fluid (normal volume is 3-5 ml)[7].
Arterial calcification
Arterial calcification can be caused by high serum calcium-phosphate levels in CKD patients. One study of 96 patients, aged 18–70 found coronary calcification in 64%, and severe calcification present in 23% of patients.
Using Chinese herbal formulas, Kidney Health Institute Practitioner can help CKD patients to address their cardiovascular complications successfully. For patients who have advanced heart complications, during the treatment they usually first observe an increase in blood creatinine and BUN levels, which reflects the response of the heart condition to the treatment by down-loading the toxic waste from the heart. After the heart complication is resolved, patients can achieve continual reduction in blood creatinine.
Complication of Infections
Glomerulonephritis is the 3rd leading cause of CKD. CKD patients are also more prone to infection because of related conditions such as diabetes, or inadequate calorie and protein intake. Chronic infections can cause damage and scarring to the kidney leading to accelerated kidney degeneration. A suppressed immune system in CKD patients due to uremia results in an increase in susceptibility to infections. Around 48% of deaths in CKD patients are associated with these infections.
Infection by atypical bacterial infections such as mycoplasma pneumoniae and Chlamydia pneumoniae is common among CKD patients. IgA nephropathy has been found to associate with Mycoplasma pneumonia infections [8].
Using Chinese herbal formulas, Kidney Health Institute Practitioners can help CKD patients to reduce these infections effectively.
- With 2-4 weeks of treatment, patients can experience improvement in infection related symptom
- With 4-6 weeks of treatment, patients can have significant improvement with sustained results.
Selected Practitioners View All Practitioner
View All Practitioner
If you have any questions, please click here to contact us for further information.
References
[1] Tedla FM, Brar A, et al, Hypertension in Chronic Kidney Disease: Navigating the Evidence. Int J Hypertens. 2011; 2011: 132405
[2] O’Mara NB, Anemia in Patients With Chronic Kidney Disease. Diabetes Spectrum. January 2008 vol. 21 no. 112-19
[3] Sampanis CH, Management of hyperglycemia in patients with diabetes mellitus and chronic renal failure. Hippokratia. 2008 Jan-Mar; 12(1): 22–27.
[4] Silverberg D1, Wexler D, et al. The association between congestive heart failure and chronic renal disease. Curr Opin Nephrol Hypertens. 2004 Mar;13(2):163-70.
[5] Bailay GL, Hampers CL, Uremic Pericarditis: Clinical Features and Management. Circulation. 1968;38:582-591
[6] Kabukcu M, Demircioglu F, et al, Pericardial Tamponade and Large Pericardial Effusions. Tex Heart Inst J. 2004; 31(4): 398–403.
[7] Kleiman JH, Motta J, et al, Pericardial effusions in patients with end-stage renal disease. Br Heart J. 1978 Feb; 40(2): 190–193.
[8] Kashyap S and Sarkar M, Mycoplasma pneumonia: Clinical features and management. Lung India. 2010 Apr-Jun; 27(2): 75–85.
